Abstract
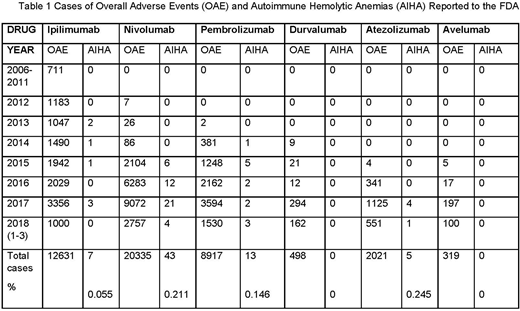
Immune checkpoint inhibitors (CPI) are widely used in modern oncology and have improved the prognosis of lung cancer, bladder cancer, malignant melanoma and other malignancies. Unlike cytotoxic chemotherapy, drugs like nivolumab, pembrolizumab and ipilimumab are associated with a high frequency of immune-related adverse effects. We recently observed a patient with lung cancer who developed a fulminant warm-antibody autoimmune hemolytic anemia (AIHA) and reviewed the literature and public databases of the Food and Drug Administration (FDA) to help understand the association between CPI use and AIHA. A total of 68 cases of AIHA were identified in the FDA database during the time period 2012-2018; 43 associated with nivolumab, 13 with pembrolizumab, 7 with ipilimumab and 5 with atezolizumab administration (see Table 1). All episodes of AIHA were listed as serious. If the total number of adverse effect cases reported to the FDA is taken as a reference, AIHA is rare, but occurred more frequently with PD-1 or PDL1 targeting agents (0.15 to 0.25%) than with CTLA4-inhibitors (0.06%). The underlying cancer diagnoses corresponded mostly to the approved indications for CPI (32 cases of malignant melanoma, 24 cases of lung cancer). In about a quarter of cases with AIHA other immune related side effects were reported. In addition to our case, the literature review identified 10 similar cases. AIHA can occur earlier and later after the administration of CPI (median of 10 weeks, range 2- 78). Most cases of AIHA responded to steroids, but 2/11 were fatal. In conclusion, we describe AIHA as a rare and serious immune-related side effect of checkpoint inhibitors. Because of its seriousness and the underlying comorbidities, early aggressive management is necessary.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal